Total parenteral nutrition (TPN)
A look at TPN
TPN is a highly concentrated, hypertonic nutrient solution administered by way of an infusion pump through a large central vein. For patients with high caloric and nutritional needs due to illness or injury, TPN provides crucial calories, restores nitrogen balance, and replaces essential fluids, vitamins, electrolytes, minerals, and trace elements. TPN also promotes tissue and wound healing and normal metabolic function; gives the bowel a chance to heal; reduces activity in the gallbladder, pancreas, and small intestine; and is used to improve a patient’s response to surgery.
Patients who can’t meet their nutritional needs by oral or enteral feedings may require I.V. nutritional supplementation or TPN. Generally, this treatment is prescribed for any patient who can’t absorb nutrients from the GI tract for more than 10 days. More specific indications include:
- debilitating illnesses lasting longer than 2 weeks
- loss of 10% or more of pre-illness weight
- serum albumin level below 3.5 g/dl
- excessive nitrogen loss from a wound infection, a fistula, or an abscess
- renal or hepatic failure
- nonfunction of the GI tract lasting for 5 to 7 days .
Understanding common TPN additives
Common components of total parenteral nutrition (TPN) solutions such as glucose, amino acids, and other additives are used for specific purposes. For instance, glucose provides calories for metabolism. Here’s a list of other common additives and the purposes each serves.
- Electrolytes
- Vitamins
- Other additives
- Calcium promotes development and maintenance of bones and teeth and aids in blood clotting .
- Chloride regulates acid-base balance and maintains osmotic pressure .
- Magnesium helps the body absorb carbohydrates and protein .
- Phosphorus is essential for cell energy and calcium balance .
- Potassium is needed for cellular activity and cardiac function .
- Sodium helps control water distribution and maintains normal fluid balance .
- Folic acid is needed for deoxyribonucleic acid (DNA) formation and promotes growth and development.
- Vitamin B complex helps the final absorption of carbohydrates and protein.
- Vitamin C helps in wound healing.
- Vitamin D is essential for bone metabolism and maintenance of serum calcium levels.
- Vitamin K helps prevent bleeding disorders.
- Micronutrients (such as zinc, copper, chromium, selenium, and manganese) help in wound healing and red blood cell synthesis.
- Amino acids provide the proteins necessary for tissue repair and immune functions.
- Lipids support hormone and prostaglandin synthesis and prevent essential fatty acid deficiency.

TPN triggers
Common illnesses or treatments that can trigger the need for TPN include inflammatory bowel disease, ulcerative colitis, bowel obstruction or resection, radiation enteritis, severe diarrhea or vomiting, acquired immunodeficiency syndrome (AIDS), chemotherapy, and severe pancreatitis, all of which hinder a patient’s ability to absorb nutrients. Also, patients may benefit from TPN if they’ve undergone major surgery or if they have a high metabolic rate resulting from sepsis, trauma, or burns of more than 40% of total body surface area. Infants with congenital or acquired disorders may need TPN to promote proper growth and development.
TPN has limited value for well-nourished patients with GI tracts that are healthy or are likely to resume normal function within 10 days. The treatment also may be inappropriate for a patient with a poor prognosis or when the risks of TPN outweigh its benefits.
Peripheral parenteral nutrition (PPN) is prescribed for patients who have a malfunctioning GI tract and need short-term nutrition lasting less than 2 weeks. It may be used to provide partial or total nutitional support. PPN is infused peripherally in various combinations of lipid (fat) emulsions and amino acid-dextrose solutions. To ensure adequate nutrition, PPN solutions in final concentratons of ≤ ۱۰% dextrose and ≤ ۵% protein shouldn’t be administered for longer than 10 days unless they’re supplemented with oral or enteral feedings.
The trend of today’s nutritional supplementation is to tailor TPN formulas to the patient’s specific needs. As a result, standard TPN mixtures are becoming less popular. Nutritional support teams consisting of nurses, doctors, pharmacists, and dietitians assess, prescribe for, and monitor patients receiving TPN. The solutions may consist of:
- protein (essential and nonessential amino acids), with varying types available for patients with renal or liver failure
- dextrose (10% to 35% concentration)
- fat emulsions (20% to 30% solution)
- electrolytes
- vitamins
- trace element mixtures .
Lipid emulsions
Lipid emulsions are thick emulsions that supply patients with both essential fatty acids and calories. These emulsions assist in wound healing, red blood cell (RBC) production, and prostaglandin synthesis. They may be piggybacked with TPN, given alone through a separate peripheral or central venous line, or mixed with amino acids and dextrose in one container (total nutrient admixtures) and infused over 24 hours.
Lipid emulsions should be given cautiously to patients with hepatic or pulmonary disease , acute pancreatitis , anemia , or a coagulation disorder and to patients at risk for developing a fat embolism . These emulsions shouldn’t be given to patients who have conditions that disrupt normal fat metabolism, such as pathologic hyperlipidemia, or lipid nephrosis.
Also, make sure you report any adverse reactions to the practitioner so the TPN regimen can be changed as needed.
Adverse reactions to lipid emulsions : Lipid emulsions can cause immediate adverse reactions as well as delayed complications.
- Back and chest pain
- Cyanosis
- Diaphoresis or flushing
- Dyspnea
- Headache
- Hypercoagulability
- Irritation at the site
- Lethargy or syncope
- Nausea or vomiting
- Slight pressure over the eyes
- Thrombocytopenia
- Blood dyscrasias
- Fatty liver syndrome
- Hepatomegaly
- Jaundice
- Splenomegaly
How to infuse TPN
TPN must be infused through a central vein. As a hypertonic solution, it may be up to six times the concentration of blood and, therefore, too irritating for a peripheral vein.
TPN may be infused around the clock or for part of the day for instance, as the patient sleeps at night. A sterile catheter made of polyurethane or silicone is inserted into the subclavian or jugular vein. A polyurethane catheter is rigid during insertion but softens at body temperatue. It’s biocompatible, so tissues don’t react to the material and it’s less thrombogenic than earlier types of manufactured catheters. A Silastic catheter may be a better alternative for therapy lasting months or years because it’s more flexible and durable and it’s compatible with many medications and solutions.
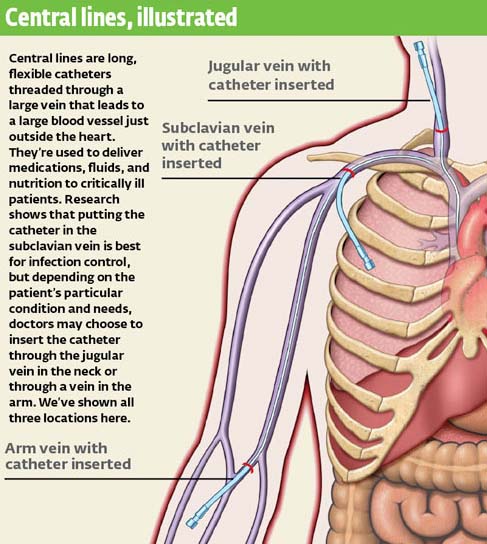
Looking to the peripheral
A peripherally inserted central catheter, a variation of central venous therapy, can be used for therapy lasting 3 months or more. The catheter is inserted through the basilic or cephalic vein and threaded so that the tip lies in the superior vena cava.
The patient generally experiences less discomfort with a peripheral catheter, especially if he can move around easily. Movement stimulates blood flow and decreases the risk of phlebitis. Peripherally inserted central catheters are often used for intermediate-term therapy, both at home and in the health care facility.
Signs and symptoms of electrolyte imbalances caused by TPN administration include abdominal cramps, lethargy, confusion, malaise, muscle weakness, tetany, convulsions, and cardiac arrhythmias. Acid-base imbalances can also occur as a result of the patient’s condition or the TPN content. Look for these other complications:
- heart failure or pulmonary edema from fluid and electrolyte administration, conditions that can lead to tachycardia, lethargy, confusion, weakness, and labored breathing
- hyperglycemia from dextrose infusing too quickly, a condition that may require an adjustment in the patient’s insulin dosage
- adverse reactions to medications added to TPN for example, added insulin can cause hypoglycemia, which can result in confusion, restlessness, lethargy, pallor, and tachycardia
- catheter-related infections and catheter occlusion.
Constant assessment and rapid intervention are critical for patients receiving TPN. When caring for a patient receiving TPN, you’ll want to take these actions:
- Carefully monitor patients receiving TPN to detect early signs of complications, such as infection, metabolic problems, heart failure, pulmonary edema, or allergic reactions. Adjust the TPN regimen as needed.
- Assess the patient’s nutritional status, and weigh the patient at the same time each morning in similar clothing, after he voids, and on the same scale. Weight indicates nutritional progress and also determines fluid overload. Patients ideally should gain 1 to 2 lb (0.5 to 1 kg)/week. Weight gain greater than 1 lb (0.5 kg)/day indicates fluid retention.
- Assess the patient for peripheral and pulmonary edema. Edema is a sign of fluid overload.
Teaching about TPN When teaching a patient about total parenteral nutrition (TPN), be sure to cover the following topics and then evaluate your patient’s learning:
- basics of TPN and its specific use
- adverse reactions or catheter complications and when to report them
- basic care of a TPN line
- maintenance of equipment
- weight, calorie count, intake and output, and glucose level monitoring.
The sugar situation
- Monitor serum glucose levels every 6 hours initially, then once a day. Watch for thirst and polyuria, which are indications that the patient may have hyperglycemia. Periodically confirm glucometer readings with laboratory test results. Serum glucose levels should be less than 200 mg/dl. This indicates the patient’s tolerance of the glucose solution.
- Monitor for signs and symptoms of glucose metabolism disturbance, fluid and electrolyte imbalances, and nutritional problems. Some patients may require insulin added directly to the TPN for the duration of treatment.
- Monitor electrolyte levels daily at first, and then twice a week. Keep in mind that when a patient is severely malnourished, starting TPN may spark refeeding syndrome, which includes a rapid drop in potassium, magnesium, and phosphorus levels. To avoid compromising cardiac function, initiate feeding slowly and monitor the patient’s electrolyte levels closely until they stabilize.
- Monitor protein levels twice a week. Albumin levels may drop initially as treatment restores hydration.
- Check renal function by monitoring blood urea nitrogen (BUN) and creatinine levels; increases may indicate excess amino acid intake.
- Assess nitrogen balance with 24-hour urine collection.
- Assess liver function with liver function tests, bilirubin, triglyceride, and cholesterol levels. Abnormal values may indicate intolerance.
- Review the patient’s serum chemistry and nutritional studies, and alert the practitioner of abnormal results, which may indicate that the TPN fluid concentration or ingredients may need to be adjusted to meet the patient’s specific needs.
- Avoid an adverse reaction by starting TPN slowly usually 60 to 80 ml/hour for the first 24 hours and increasing gradually. Continually monitor the patient’s cardiac and respiratory status.
- Use an infusion pump for rate control.
To remember how to avoid the complication of refeeding syndrome when giving total parenteral nutrition to a severely malnourished patient, think “Start low and go slow.”
Documenting TPN : If your patient is receiving total parenteral nutrition, make sure you document the following information:
Total parenteral nutrition review (کلیک کنید )
- Highly concentrated, hypertonic nutrient solution used for patients with high caloric and nutritional needs due to illness or injury
- Provides crucial calories, restores nitrogen balance, and replaces essential fluids, vitamins, electrolytes, minerals, and trace elements
- Promotes tissue and wound healing and normal metabolic function; gives the bowel a chance to heal; reduces activity in the gallbladder, pancreas, and small intestine; and improves a patient’s response to surgery
- Used in patients who can’t meet their nutritional needs by oral or enteral feedings, including those with inflammatory bowel disease, ulcerative colitis, bowel obstruction or resection, radiation enteritis, severe diarrhea or vomiting, AIDS, chemotherapy, and severe pancreatitis
- Typically has limited value in well-nourished patients with GI tracts that are healthy or are likely to resume normal function within 10 days
- Must be infused through a central vein
Common TPN additives
- Electrolytes
- Vitamins
- Other additives
- Lipid emulsions
- Calcium: promotes development and maintenance of bones and teeth and aids in blood clotting
- Chloride: regulates acid-base balance and maintains osmotic pressure
- Magnesium: helps the body absorb carbohydrates and protein
- Phosphorus: essential for cell energy and calcium balance
- Sodium: helps control water distribution and maintains normal fluid balance
- Folic acid: helps with DNA formation and promotes growth and development
- Vitamin B complex: helps the final absorption of carbohydrates and protein
- Vitamin C: helps in wound healing
- Vitamin D: essential for bone metabolism and maintenance of serum calcium levels
- Vitamin K: helps prevent bleeding disorders
- Micronutrients (zinc, copper, chromium, selenium, manganese): help in wound healing and red blood cell synthesis
- Amino acids: provide the proteins necessary for tissue repair and immune functions
- Lipids: support hormone and prostaglandin synthesis; prevent essential fatty acid deficiency
- Thick preparations that supply patients with essential fatty acids and calories
- Assist in wound healing, RBC production, and prostaglandin synthesis
- May be piggybacked with TPN
- Should be used cautiously in patients with hepatic or pulmonary disease, acute pancreatitis, anemia, or a coagulation disorder and in patients at risk for developing a fat embolism
- Should be avoided in patients with pathologic hyperlipidemia or lipid nephrosis
- Electrolyte imbalances
- Acid-base imbalances
- Heart failure or pulmonary edema
- Hyperglycemia
- Rebound hypoglycemia
- Refeeding syndrome (in severely malnourished patients), which includes a rapid drop in potassium, magnesium, and phosphorus levels
- Assess nutritional status and daily weight.
- Assess for edema, a sign of fluid overload.
- Monitor serum glucose level every 6 hours initially, then once daily.
- Monitor electrolyte levels daily at first, then twice weekly.
- Monitor protein levels twice weekly.
- Monitor BUN and creatinine levels, liver function tests, and nitrogen balance
Fluids & Electrolytes made Incredibly Easy ! ®, ۵th Edition
Copyright ©۲۰۱۱ Lippincott Williams & Wilkins
تهیه و تنظیم : صادق دهقانی زاده
 the nursing station ایستگاه پرستاری
the nursing station ایستگاه پرستاری






سلام پایگاه پرستاری
در صورتی که امکان تبادل لینک دارید ما رو به اسم “پایگاه سلامت” لینک کنید و دستور بده لینکتون کنم.
منونم از بابت زحمتی که در راه پرستاری میکشید . بروی چشم در جهت هم سو شدن فعالیت هامون شما رو لینک کردم شما هم ما رو با نام ایستگاه پرستاری لینک کنید
سلام
ممنون بخاطر زحماتی که می کشید. خسته نباشید 🙂
ما یه تیم هستیم این نتیجه کار گروهی مونه ، من هم از شما تشکر میکنم
As always, i am just motivated from the individuals on this website, especially those pals which help keep me on course often. Luna cafes and separate fowl hands and fingers in the recreation with my child but it is.
There exists this like a favourable realist folks* What exactly do you eat rather than wheat? or possibly is it merely all bad no reason to become feeding on it firstly. I’ll be executing a several launches whilst in las vegas, nevada that will convert a number of minds. If you have any inquiries concerning where and ways to make use of treadmill reviews, you could contact us at our web site.| http://findyourtreadmill.com